Understanding Anal Fistula and Why Recurrent Infections Occur
An anal fistula is an abnormal tunnel that forms between the anal canal and the surrounding skin, often developing after an abscess fails to heal completely. This tunnel allows bacteria to travel repeatedly between internal tissue and the outer skin, creating a cycle of infection that can be difficult to break without medical intervention. Many people experience temporary relief when drainage occurs, but the underlying tract remains, making reinfection likely. Recurrent infections happen because the fistula continues to harbor bacteria even when symptoms temporarily subside. Over time, repeated inflammation can cause the tract to widen or branch, making treatment more complex. Ignoring symptoms or relying solely on home remedies often worsens the condition. Understanding how and why these infections persist helps patients recognize the importance of proper anal fistula repair and removal for long term relief.
Signs and Symptoms That Point to Chronic or Recurrent Infection
Recurrent anal fistula infections often present with a predictable pattern of discomfort that disrupts daily life. Persistent pain near the anus is common, especially when sitting or during bowel movements. Many patients notice swelling or redness that comes and goes as infections flare and drain. Discharge of pus or blood is another key sign, often accompanied by an unpleasant odor that causes embarrassment and skin irritation. Fever or fatigue may appear during active infection, signaling that the body is fighting inflammation. Itching and moisture around the anal area can worsen over time, leading to secondary skin problems. Recognizing these ongoing symptoms early can help prevent complications and prompt timely evaluation for anal fistula repair and removal.
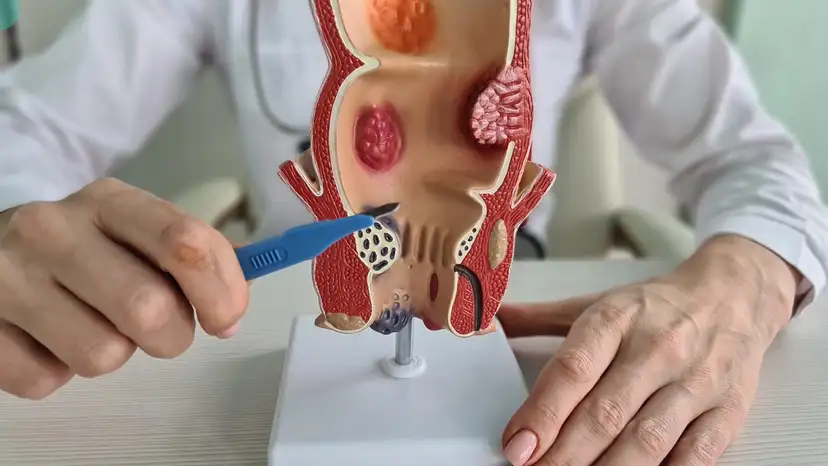
Medical Evaluation and Diagnostic Methods for Anal Fistula
Accurate diagnosis plays a vital role in managing recurrent infections effectively. A healthcare provider typically begins with a detailed medical history and physical examination to assess visible openings and drainage. Imaging studies such as magnetic resonance imaging or specialized ultrasound are often used to map the fistula tract beneath the skin. These tools help identify branching tunnels and their relationship to the sphincter muscles. Proper classification ensures that treatment addresses the entire tract rather than just surface symptoms. Without thorough evaluation, parts of the fistula may remain untreated, increasing the risk of recurrence. A careful diagnostic approach allows surgeons to plan anal fistula repair and removal with greater precision and safety.
Why Anal Fistula Repair and Removal Is Necessary for Recurrent Infections
Repeated infections indicate that conservative measures alone are not enough to resolve the condition. Antibiotics may temporarily reduce inflammation, but they do not eliminate the fistula tract itself. Continued infection can lead to tissue damage, scarring, and worsening pain. Over time, untreated fistulas can affect nearby muscles, increasing the risk of bowel control issues. Chronic infection may also impact emotional wellbeing, causing stress and social withdrawal. Definitive anal fistula repair and removal aim to eliminate the source of infection rather than manage symptoms alone. Addressing the root cause helps restore comfort, confidence, and long term health.
Types of Anal Fistula Repair and Removal Procedures
Treatment options vary depending on the complexity and location of the fistula. Some procedures focus on opening the tract to allow healing from the inside out, while others involve removing the tract entirely. The primary goal is to clear infection while protecting surrounding muscles. Common approaches include surgical opening, excision, or techniques that preserve muscle function. Each method has specific benefits and recovery considerations. Selecting the right approach requires individualized assessment and surgical expertise. Understanding these options helps patients feel informed and confident about their care.
Fistulotomy as a Common Surgical Option
Fistulotomy involves opening the fistula tract along its length so it can heal naturally. This method is often recommended for simpler fistulas that do not involve much muscle tissue. By allowing the tract to remain open, bacteria are less likely to become trapped, reducing infection risk. Healing typically occurs gradually as new tissue forms from the base upward. Pain is usually manageable with proper postoperative care and hygiene. Many patients experience significant relief from recurrent infections after this procedure. Fistulotomy remains one of the most effective options for anal fistula repair and removal when anatomy allows.
Fistulectomy and Complete Tract Removal
Fistulectomy focuses on removing the entire fistula tract rather than opening it. This approach may be chosen when the tract is well defined and accessible. Removing the tract completely can reduce the chance of recurrence in certain cases. However, healing may take longer due to the larger wound area. Surgeons carefully evaluate surrounding tissue to minimize impact on muscle control. Proper wound care and follow up are essential for optimal recovery. Fistulectomy offers another reliable path to resolving recurrent infections when performed by experienced specialists.
Sphincter Preserving Techniques for Complex Cases
In more complex cases, preserving muscle function becomes a priority. Sphincter preserving techniques aim to treat the fistula without cutting critical muscles. These methods may involve staged procedures that allow gradual healing. They are often recommended for fistulas that pass through deeper muscle layers. While recovery may be longer, the focus remains on maintaining bowel control. Advances in surgical methods have improved outcomes for these challenging cases. Such approaches highlight the importance of individualized anal fistula repair and removal strategies.
Preparing for Anal Fistula Repair and Removal
Preparation helps ensure a smoother surgical experience and recovery. Patients typically undergo preoperative evaluations to assess overall health. Managing active infection before surgery may involve drainage or medication. Clear instructions regarding diet, bowel preparation, and medications are provided. Understanding what to expect reduces anxiety and improves cooperation with care plans. Open communication with the surgical team allows concerns to be addressed early. Proper preparation sets the stage for successful anal fistula repair and removal.
Recovery Timeline and Post Procedure Care
Recovery varies depending on the chosen procedure and individual healing capacity. Most patients experience gradual improvement in pain and drainage over several weeks. Keeping the area clean and dry supports healing and reduces infection risk. Dietary adjustments that promote soft bowel movements are often recommended. Regular follow up appointments help monitor progress and address concerns. Patients are encouraged to avoid straining during recovery. Consistent care and patience play key roles in achieving lasting results.
Preventing Future Infections After Surgery
Long term success depends on maintaining healthy habits after treatment. Proper hygiene helps keep the area free from bacteria. Managing bowel habits reduces pressure on healing tissue. Early recognition of unusual symptoms allows prompt intervention. Maintaining follow up care ensures that healing progresses as expected. Lifestyle choices such as balanced nutrition support tissue repair. Prevention strategies complement anal fistula repair and removal to reduce recurrence risk.
Emotional and Quality of Life Considerations
Living with recurrent infections can take a toll on emotional health. Pain, odor, and drainage often cause embarrassment and stress. Effective treatment can restore confidence and comfort in daily activities. Open discussions with healthcare providers help address fears and expectations. Support from family or trusted individuals also plays a role. Many patients report improved wellbeing after successful treatment. Addressing both physical and emotional aspects is essential for holistic recovery.
Frequently Asked Questions
What causes anal fistula to keep getting infected
Recurrent infection occurs when the fistula tract remains open and allows bacteria to persist.
Is surgery the only option for recurrent infections
Surgery is often the most effective option because it removes or opens the tract that causes infection.
How long does healing usually take
Healing time varies but often spans several weeks depending on the procedure and individual health.
Can normal activities resume after surgery
Most patients gradually return to normal activities with guidance from their healthcare provider.
Does anal fistula repair and removal prevent future problems
Proper treatment significantly reduces recurrence and improves quality of life.
Takeaway
Anal fistula repair and removal for recurrent infections focuses on eliminating the source of repeated inflammation rather than managing symptoms alone. With accurate diagnosis, appropriate surgical planning, and attentive recovery care, many individuals achieve lasting relief and restored comfort.